Communication is the Most Important Medical Instrument
Editor’s note: This guest post was written by Dave Chase, the CEO of Avado.com, a patient portal & relationship management company that was a TechCrunch Disrupt finalist. Previously he was a management consultant for Accenture’s healthcare practice and founder of Microsoft’s Health platform business. You can follow him on Twitter @chasedave.
“A good scalpel makes a better surgeon. Good communication makes a better doctor.”
- Dr. Josh Umbehr
The future of medicine in the U.S. is clear. The days of the “do more, bill more” model of reimbursement are numbered as they have produced one of the most inefficient healthcare systems in the world. While there are many unknowns regarding the future model, one thing is crystal clear — highly effective communication will separate the winners from the losers.
The quantum improvement in the depth and breadth of communication seen in the consumer Internet and in the consumerization of the enterprise (iPhones, Yammer, etc.) has yet to fully impact healthcare. With healthcare representing nearly 20% of the economy, the stakes are so high that it is inevitable that communications will be a key driver separating the winners from the losers as the tectonic shifts in the landscape shake out. This will usher in an array of new technology entrants similar to consumer and enterprise arenas disrupting ineffective and expensive communication methods of the past. The stars are aligning to make this happen.
“I don’t think you can overstate the importance of communication in clinical care. Even with devices, robotics, genomics and personalized care, it all rests, and depends on, clear communication.”
- Dr. Wendy Sue Swanson, MD, MBE, FAAP
The Individual (aka the Patient) is the Most Important Member of the Care Team
It’s long been said that the most important member of the care team is the individual (or their family member).
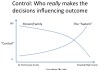
Quite simply, in a world where one is compensated on value and outcome, it’s nearly impossible to have success without recognizing the importance of the patient. Consider the diagram in this article. It is clear and appropriate that the “system” — i.e., the collection of healthcare providers — is in control of decisions that drive outcomes in high acuity cases such as when one is unconscious in the hospital. In contrast, in low acuity situations such as managing a chronic condition, the individual and/or their family are clearly in control of actions that will drive the ultimate outcome. Whether adhering to an exercise, diet or prescription plan, the patient/family plays the central role in determining the outcome.
The importance of this can’t be overemphasized given that 75% of healthcare spend results from chronic conditions. Decisions made while a condition is in low acuity can rapidly lead to high acuity flare ups that drive large medical bills. As Dr. Swanson states, “the steering wheel should be attended by the patient.” After all, 99+% of an individual’s life is spent away from healthcare providers and no one else besides them is in the driver’s seat.
It is a good thing that there has been great focus put on improving communication between healthcare professionals through standards and incentives related to the new models being driven by private and federal insurance programs. The Patient Centered Medical Home and the Accountable Care Organizations are the two most high profile of these. However, the communication focus has been about the patient not with the patient. Having worked in and seen literally hundreds of healthIT systems, the fact is the fundamental purpose of the patient as envisioned by these systems is that the “patient” is merely a vessel to attach billing codes to — not a core part of the care team. This legacy approach will prove to be a fatal flaw in the new reimbursement models. Throwing bodies (e.g., care coordinators) at the problem can help, but will be at a disadvantage versus approaches that combine the best of human and technology driven communication methods.
There are efforts being made to tweak legacy software to address these requirements. Unfortunately, they are as likely to meet the new imperatives as AOL, Microsoft and Yahoo have been at becoming market leaders in social networking. The reality is Facebook built social networking into their core design from the ground up and bolting a dramatically different approach onto an old system rarely works whether it is social networking or patient-provider communications.
Good News for Forward Looking Healthcare Organizations
I get knowing nods from my physician friends when I exclaim that I hear more frequently from my dog’s vet than my doctor or my kids’ doctor. We realize why the historical reimbursement models have contributed to this dynamic. Considering that people retain less than 20% of what a doctor tells them, this lack of communication and patient retention is a brutal combination driving sub-optimal outcomes. The good news is there is a tremendous competitive advantage that a healthcare provider can realize if they choose to focus on improved communications for the 99+% of the time when a patient isn’t staring them in the face.
Not only can this opportunity provide a competitive advantage, it is imperative in the new models. Simplistic patient portals, however, won’t get the job done. I’ve yet to meet the physician or individual who thinks that just making lab results available to patients or allowing for secure messaging is changing the care paradigm.
Whether out of desire or necessity, consumers are ready for improved communication so they can save on their healthcare costs. It’s expected that roughly one-third of the workforce will be permanent freelancers, contractors, consultants, etc. with zero expectation of employer-provided insurance. Even those with employer-provided insurance, are picking up an ever-growing percentage of the premium. The current average is 30% of the costs are picked up by an employee (up from 10% in the recent past). This coincides with the rise of consumer empowerment that has happened in virtually every other sector. Dr. Patricia Salber wrote about DIY Healthcare to explain how far things have already come and to assert her opinion that this is just the tip of the iceberg.
Thought-leading Physicians Are Ready
Fortunately the economics and simplicity of the consumer Internet and SaaS have finally come to healthcare. Once upon a time, sophisticated new software was first deployed in large enterprises. Today, greatly improved communication technologies begin with small organizations. Consider a physician like Dr. Craig Koniver who uses various free (e.g., Evernote) and low-cost off-the-shelf software to manage his communications without employing any administrative staff. Dr. Kent Bottles wrote about reverse innovation in healthcare talking about offshore innovation making its way to the U.S., but it’s not just offshore healthcare that can be a source of innovation. Dr. Howard Luks, an orthopedic surgeon, is another example of an innovative individual physician that is more sophisticated than most large healthcare providers by simply using free and low cost software to communicate with current and prospective patients.
As was highlighted in The Rise of Nimble Medicine, there is an explosion of disruptive innovators as well as innovation groups inside established healthcare organizations. In many respects, healthcare has been measured on production with an almost factory floor-like model of producing as many “widgets” (i.e., procedures, appointments, tests, prescriptions, etc.) as possible. However with a shift to a service model where success will be driven by factors such as satisfaction and health outcomes, smart healthcare providers recognize that systems optimized for production are ill-equipped to optimize for outcome. With that in mind, recognition grows that communication becomes the most important medical instrument of the future.


Leave a Reply